
We provide psychiatry education for Psychiatrists, GPs & Mental Health Practitioners.
•
Join The Academy 👇
How to get URL link on X (Twitter) App

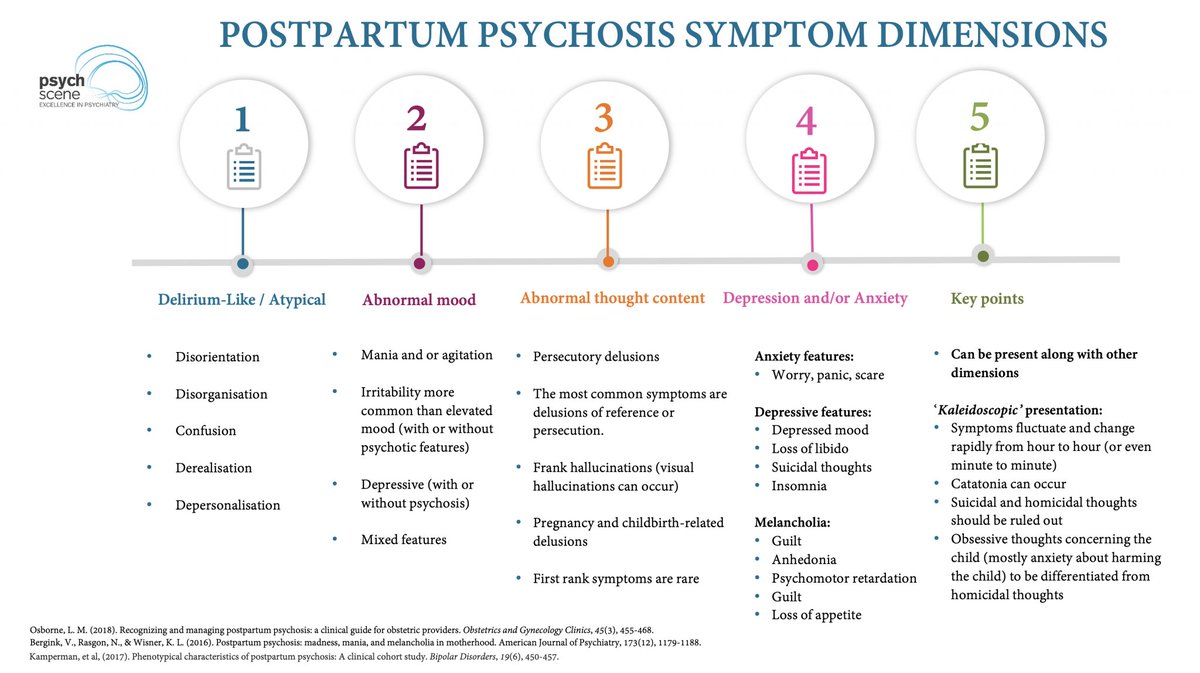
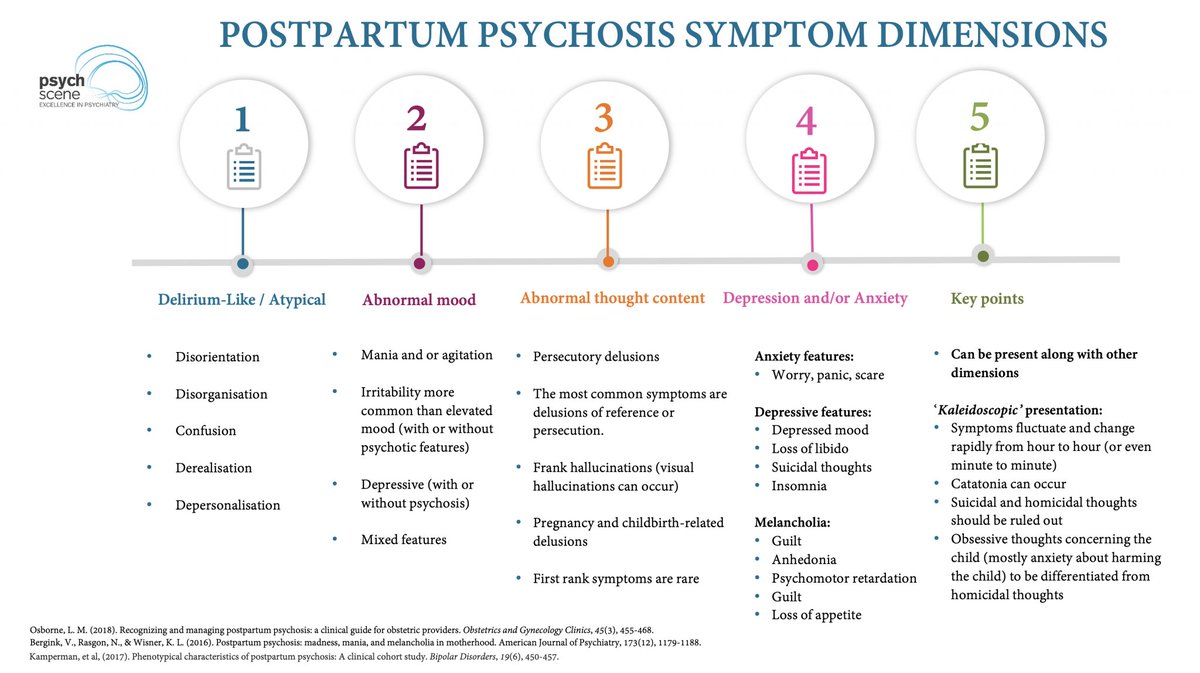 What is Postpartum Psychosis?
What is Postpartum Psychosis?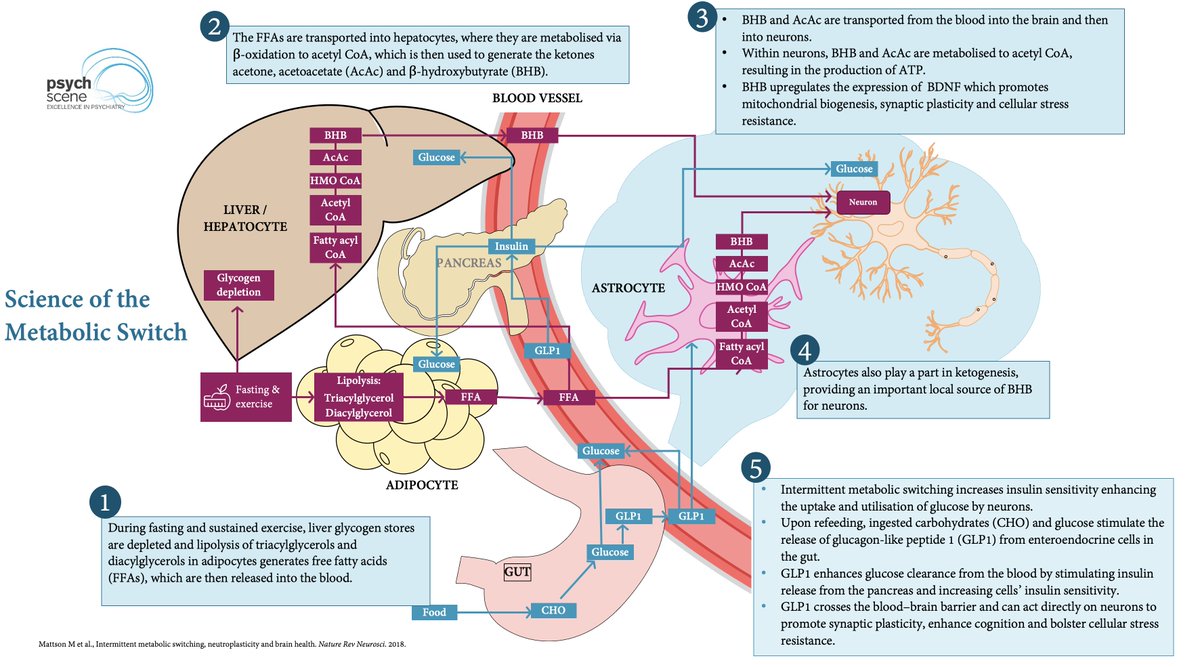
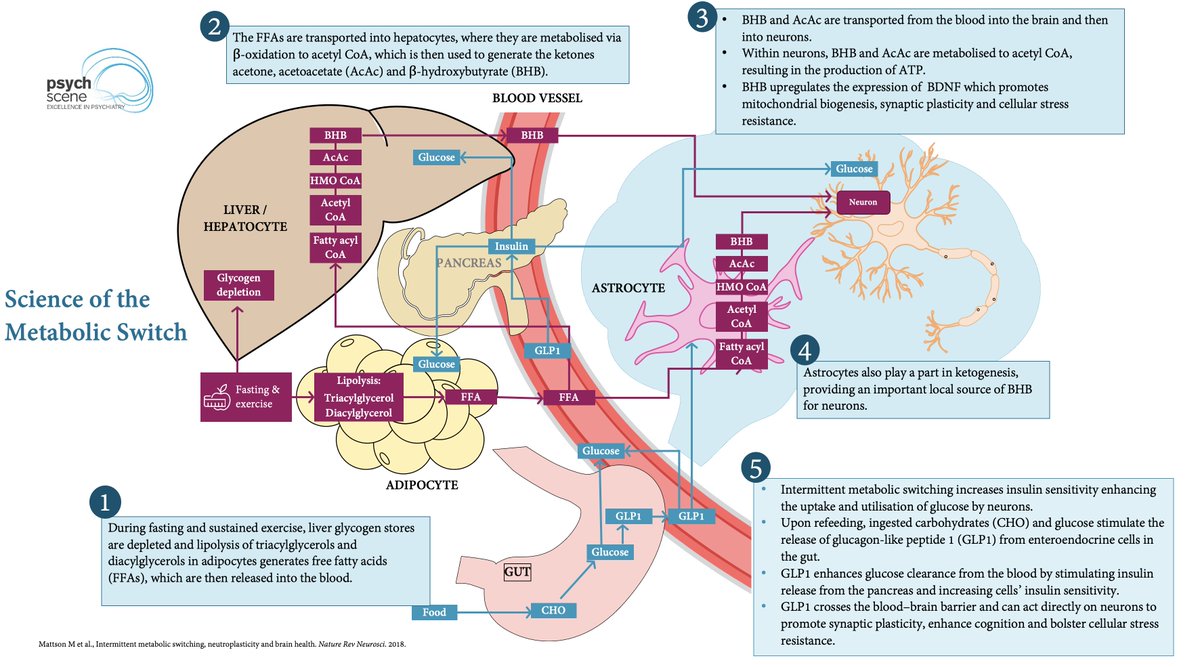 The Science Of The Metabolic Switch
The Science Of The Metabolic Switch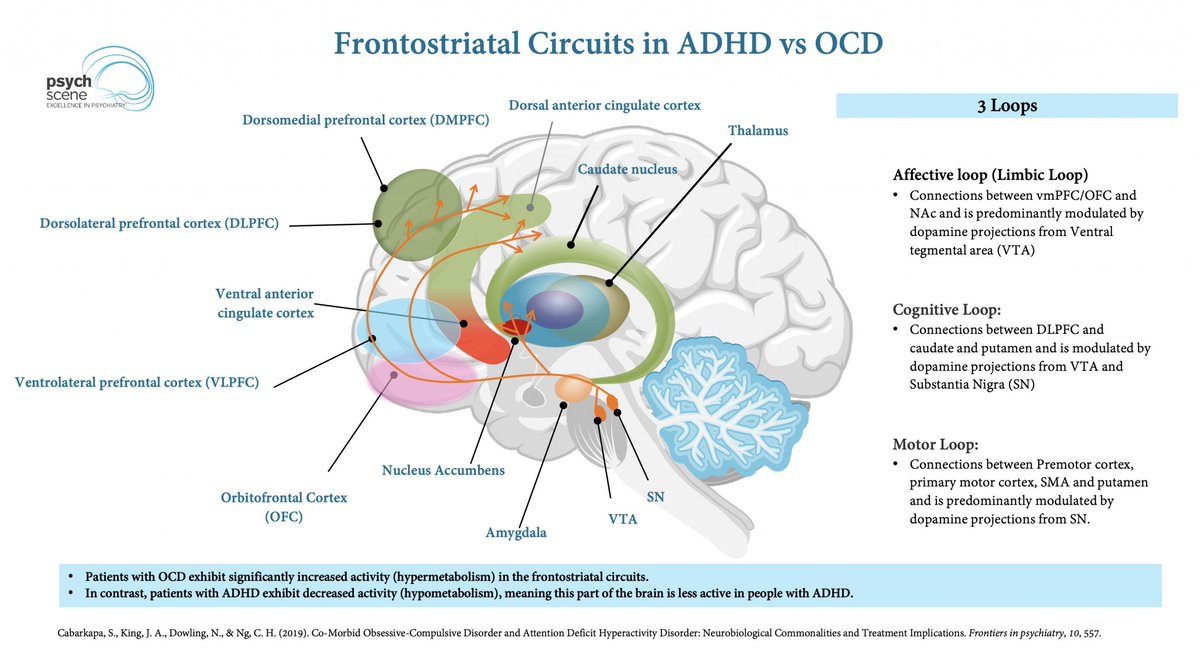
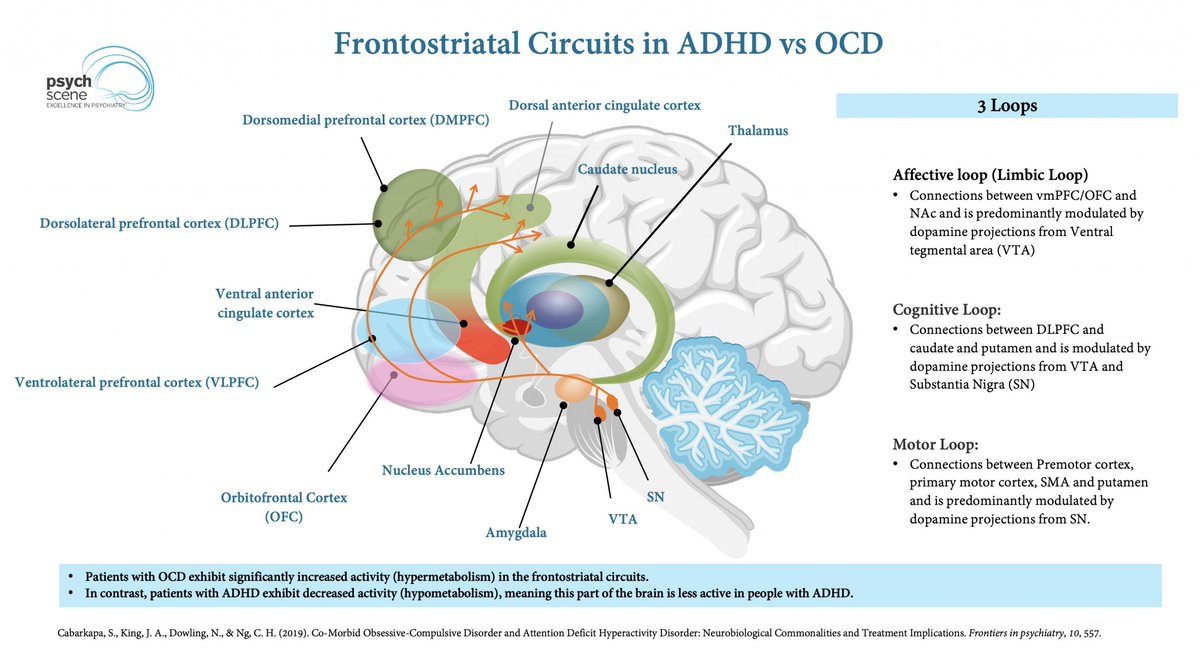 ADHD vs OCD
ADHD vs OCD
 For response rates (≥50% symptom reduction), these were the top performers:
For response rates (≥50% symptom reduction), these were the top performers: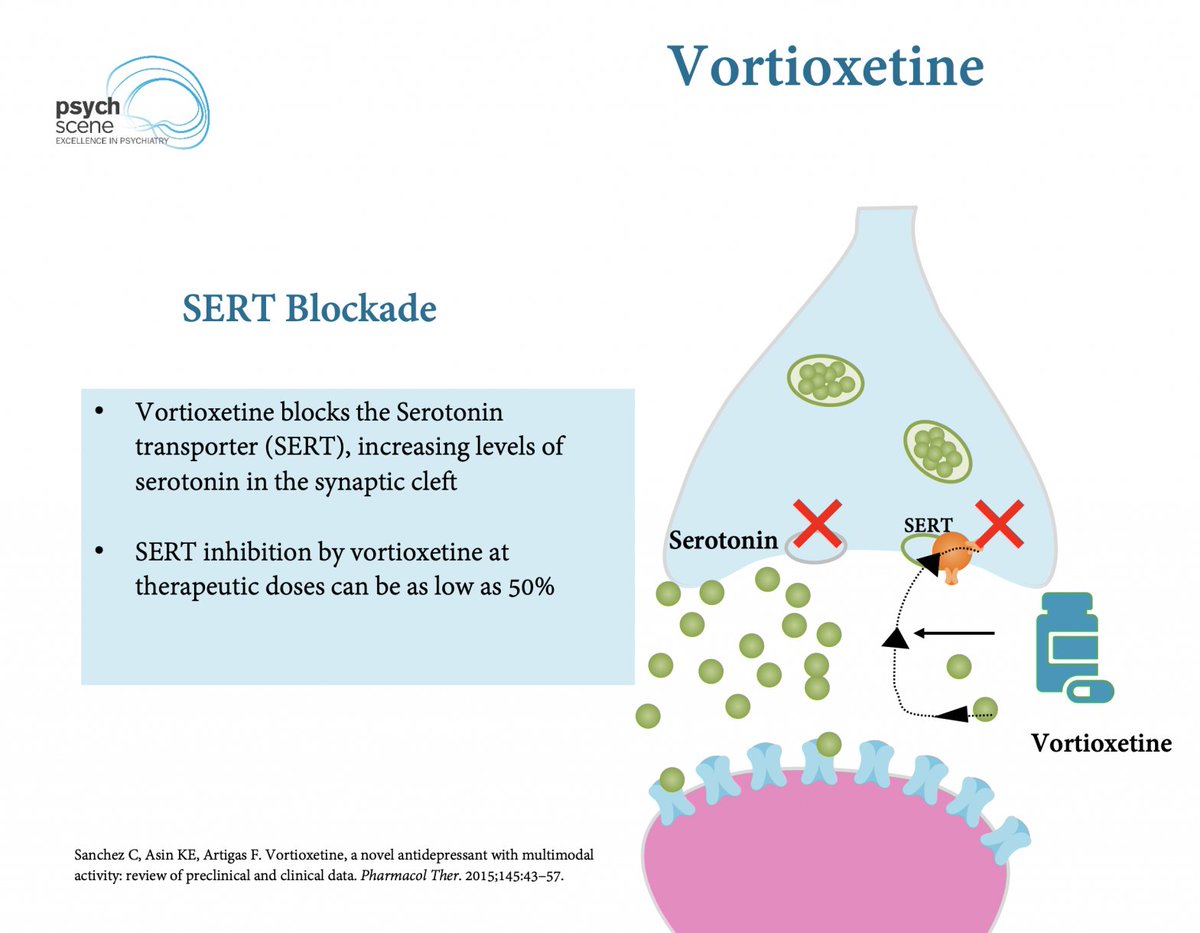
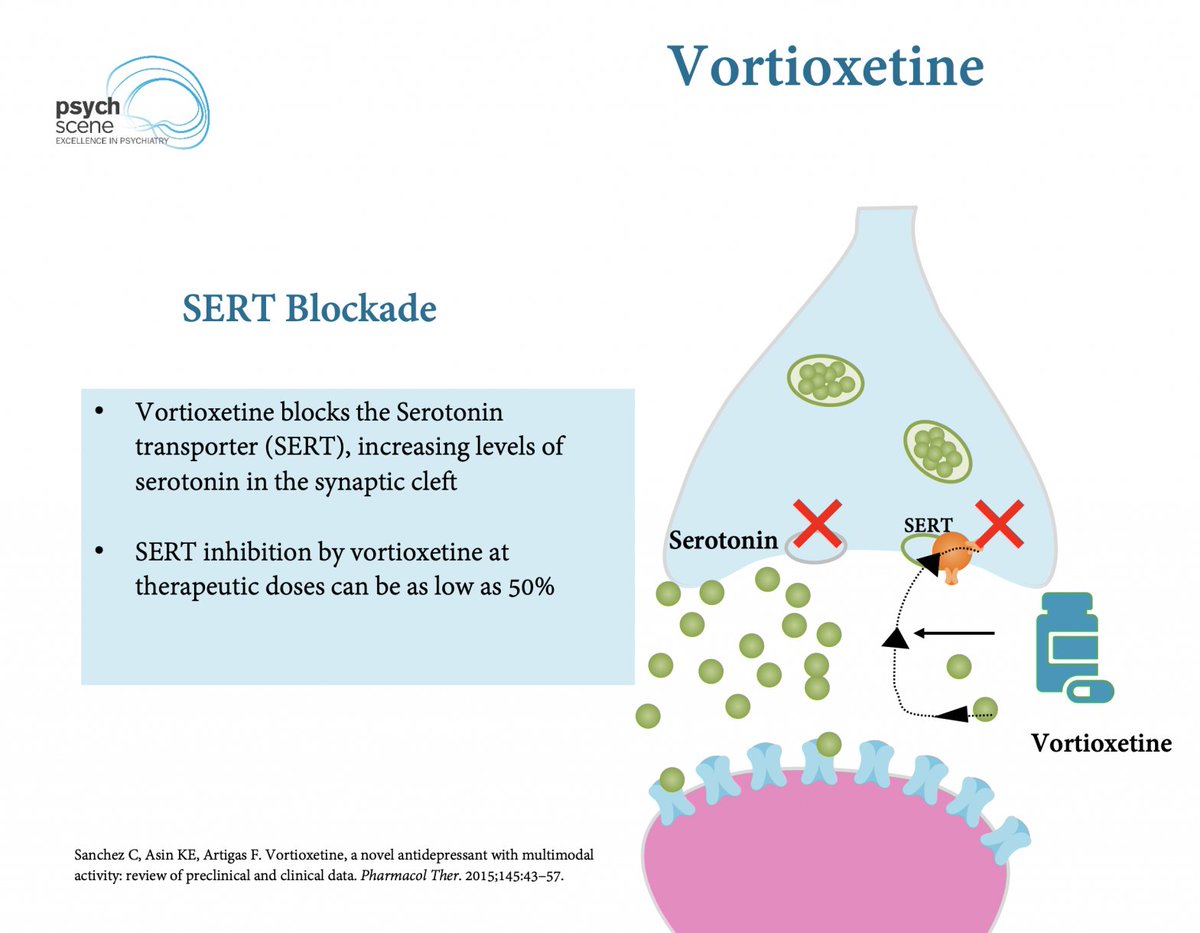 Pharmacological Profile & Multimodal Mechanism
Pharmacological Profile & Multimodal Mechanism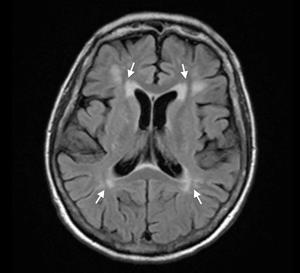
 Full Symptom Profile
Full Symptom Profile
 Stress as a Cardiovascular Risk Factor
Stress as a Cardiovascular Risk Factor
 Two PTSD Phenotypes
Two PTSD Phenotypes


 Neurobiology of Nicotine Dependence
Neurobiology of Nicotine Dependence
 The Scope of the Problem
The Scope of the Problem
 CB1 & CB2 Receptors
CB1 & CB2 Receptors
 What are Reward Prediction Errors (RPEs)?
What are Reward Prediction Errors (RPEs)?
 The Triple Network Model
The Triple Network Model

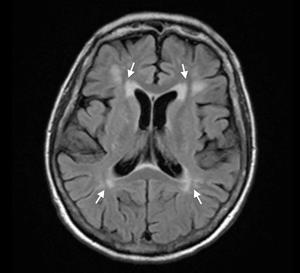
 Why Does Memantine Matter?
Why Does Memantine Matter?
 1️⃣ Understanding QTc Prolongation & TdP Risk
1️⃣ Understanding QTc Prolongation & TdP Risk
 Recognising Key Symptoms of Generalised Anxiety Disorder (GAD)
Recognising Key Symptoms of Generalised Anxiety Disorder (GAD)

 What is Anti-NMDAR Encephalitis?
What is Anti-NMDAR Encephalitis?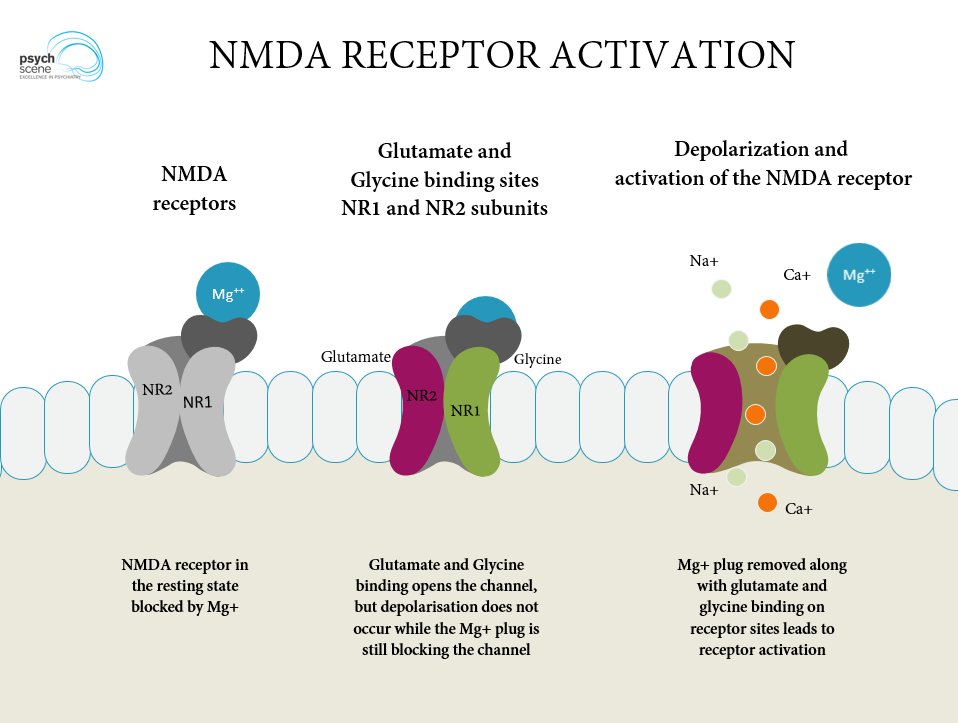
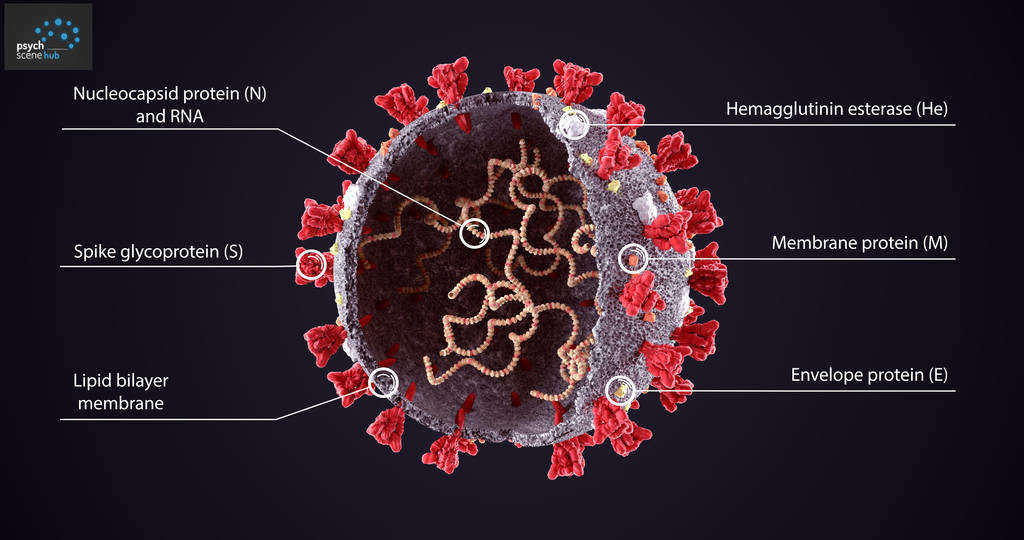 How does SARS-CoV-2 'invade' the CNS (central nervous system)?
How does SARS-CoV-2 'invade' the CNS (central nervous system)?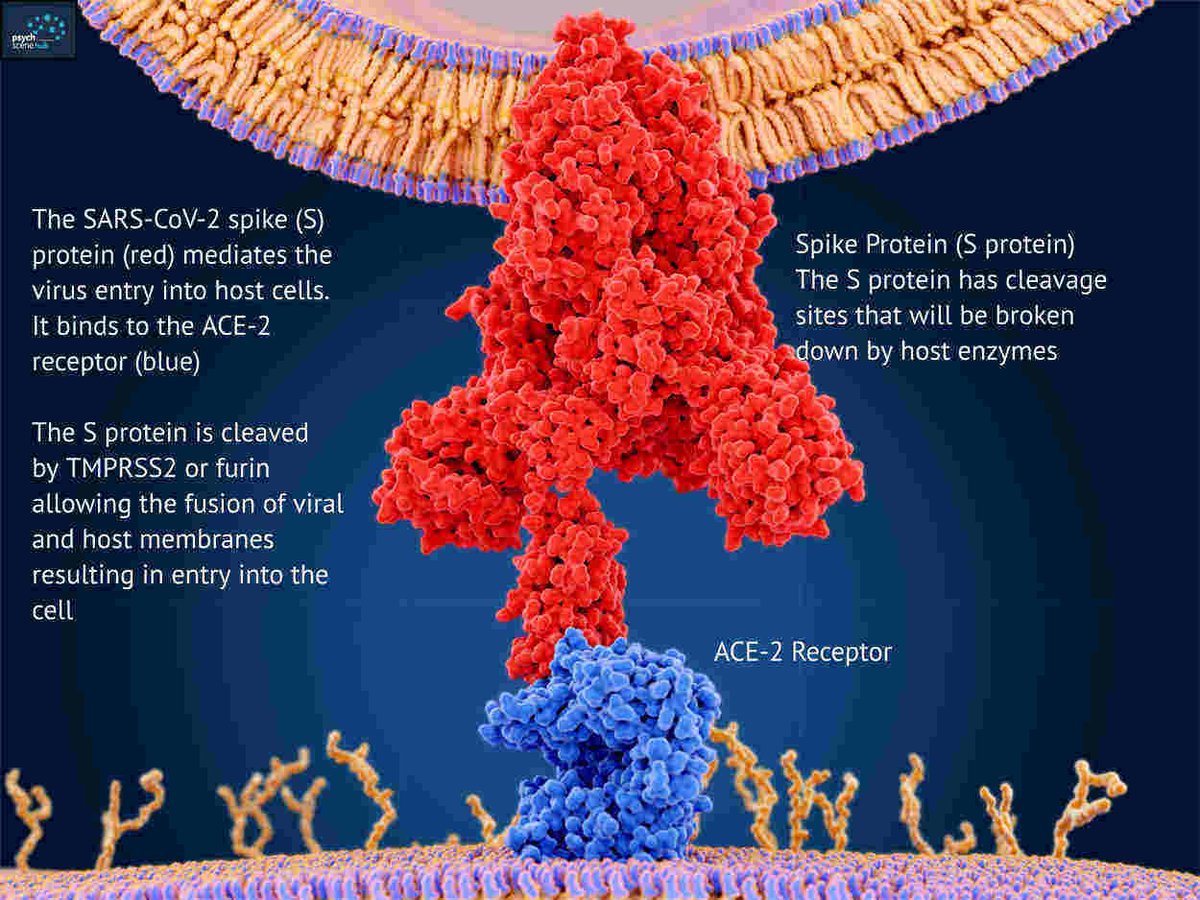
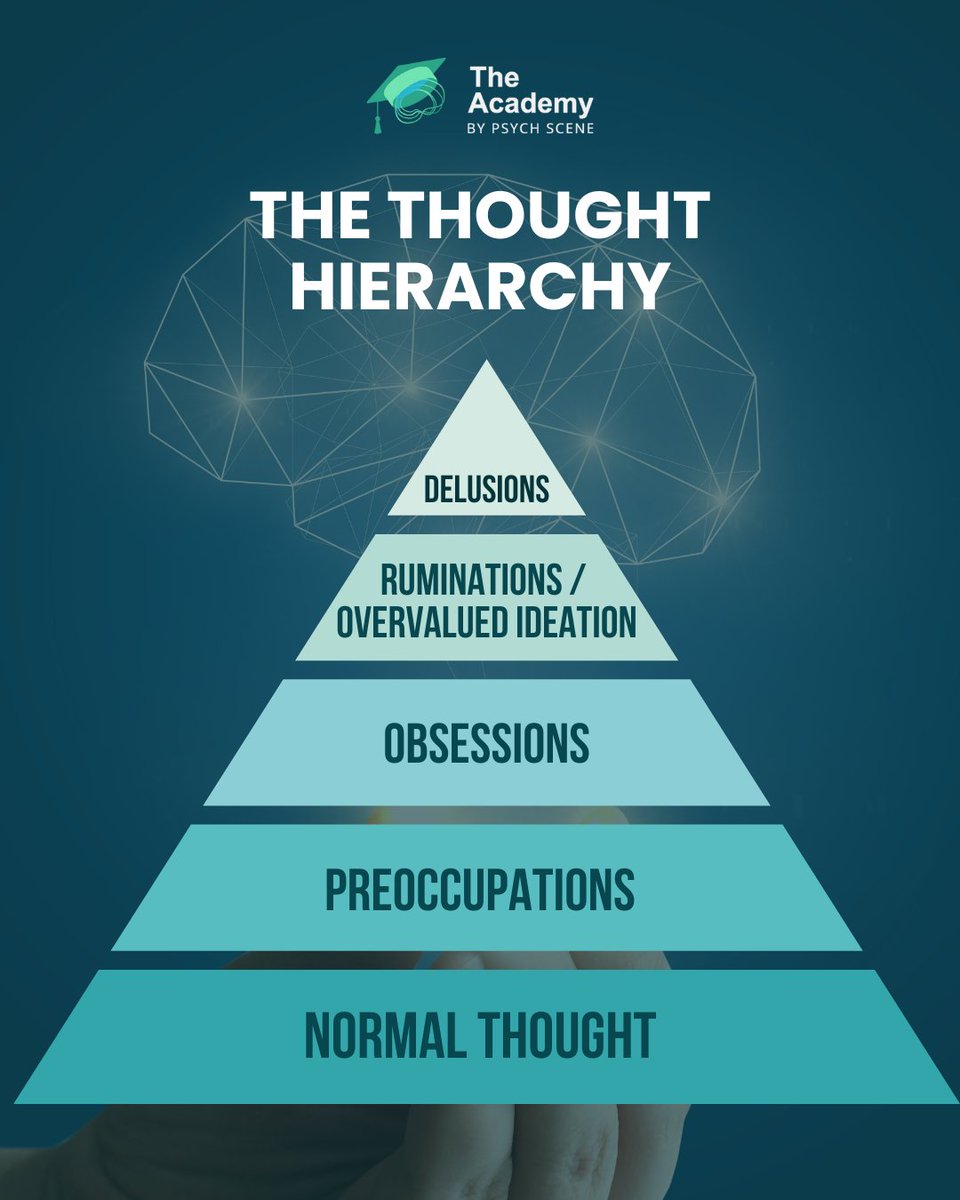
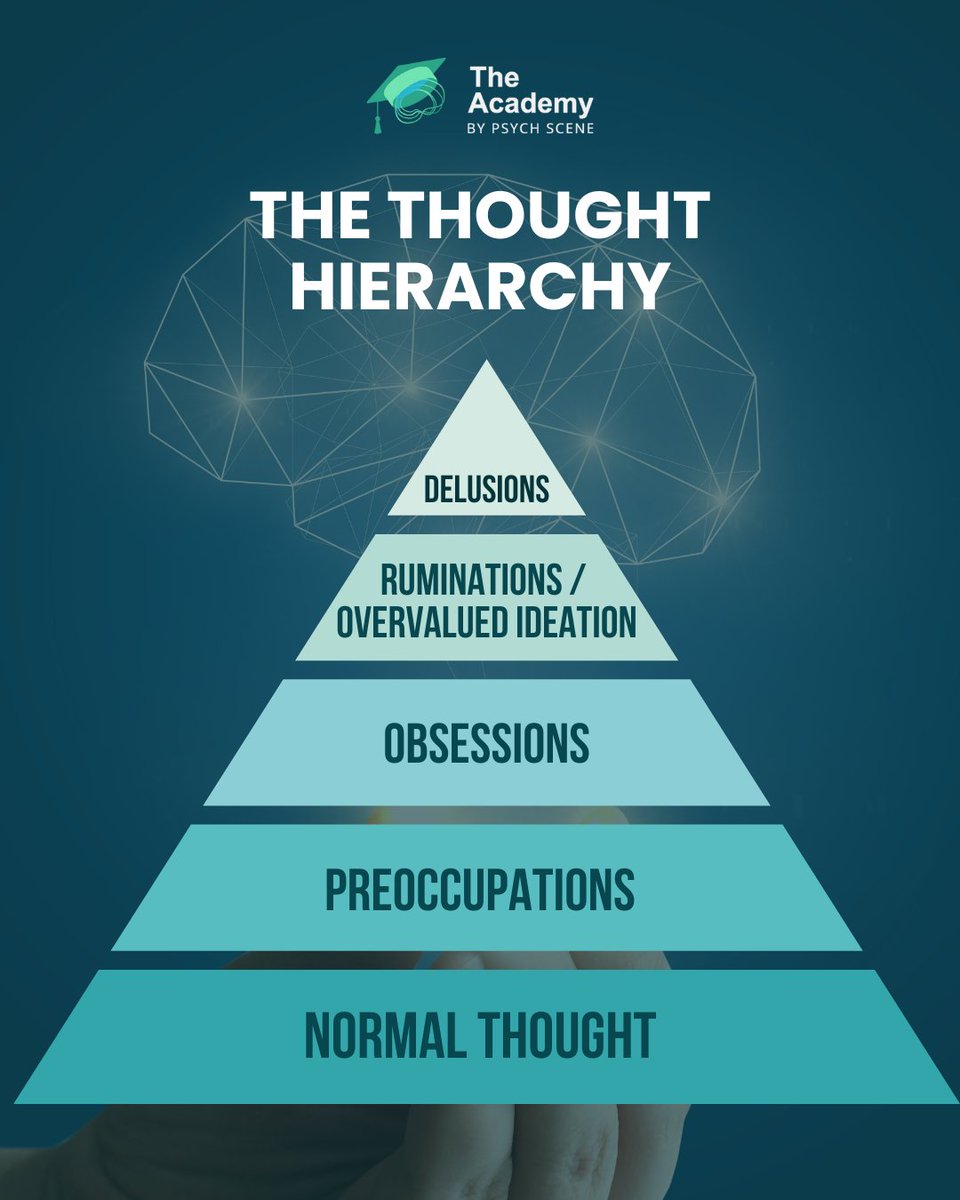 Thoughts are shaped by salience—our mind’s ability to prioritise stimuli.
Thoughts are shaped by salience—our mind’s ability to prioritise stimuli.